Why BMI Isn’t the Whole Picture: It’s Time We Rethink Health Measurements
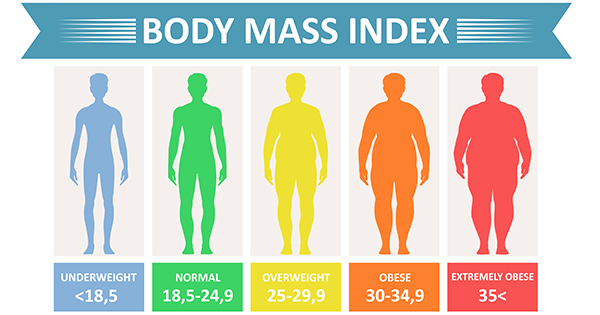
For decades, Body Mass Index (BMI) has been the go-to number for judging whether someone is underweight, “normal,” overweight, or obese. It's plastered on posters in GP surgeries, used in insurance calculations, and often brought up in health checkups.
But here’s the truth: BMI is outdated, oversimplified, and — in many cases — misleading.
A Quick History of BMI
Let’s start with a surprising fact: BMI wasn’t created as a health tool.
It was developed in the 1830s by Belgian mathematician Adolphe Quetelet — not a doctor — who was simply trying to define the "average man" for social research purposes. Fast forward a century, physiologist Ancel Keys used it to help categorise populations during large-scale cardiovascular research. It was never designed to assess individual health — and yet, somewhere along the line, we started using it that way.
No research has shown that a BMI of 24.9 is perfectly healthy, while 25 suddenly makes you unwell. And yet, health care policies, insurance companies, and even treatment access decisions are made based on this single number.
What BMI Gets Wrong
BMI only accounts for weight and height. It doesn’t care whether that weight comes from muscle or fat. It doesn’t factor in age, sex, bone density, genetics, or fat distribution. It certainly doesn’t tell us how healthy you are.
Take two people with the same BMI:
- One is a professional athlete with high muscle mass.
- The other has low muscle mass but higher levels of visceral fat (the dangerous fat around organs).
BMI treats them the same, even though their health risks may be very different.
In fact, research has shown that gynoid obesity — fat carried on the hips and thighs, often in women — may actually be protective against chronic disease. Yet many women are told to lose weight to hit an “ideal” BMI, even if it means compromising their muscle mass or hormonal health.
When a Higher BMI is Healthier
It may surprise you to hear that some research suggests having a BMI over 25 might actually be protective — especially in people over 65. A large meta-analysis published in the American Journal of Clinical Nutrition found that mortality risks only significantly increased when BMI exceeded 33 in older adults.
This is part of what’s known as the “obesity paradox” — the idea that people with a BMI in the overweight or mild obesity range sometimes have better survival outcomes in certain conditions like heart disease.
Bottom line? BMI doesn’t always reflect what’s going on beneath the surface.
What Should We Use Instead?
If BMI isn’t a good measure of health, what is?
Body Composition
Tools like bioelectrical impedance analysis (BIA) — the type used in modern body composition scales — can give us insights into fat mass, muscle mass, and hydration status. These are far more useful for tracking progress and risk factors than weight alone.
Waist-to-Height Ratio
A quick and simple metric: your waist circumference should be less than half your height. Why? Because carrying excess weight around the abdomen (visceral fat) is more closely linked to health risks than fat stored elsewhere. This measure gives us a better idea of metabolic health and cardiovascular risk.
Functional and Lifestyle Indicators
Ask yourself:
- Are you active and moving your body regularly?
- How are your energy levels, sleep, and digestion?
- Are your blood pressure, blood sugar, and cholesterol in range?
- How do your clothes fit?
These give a far clearer picture of health than a one-size-fits-all formula.
Reframing the Conversation
As clinicians, we want patients to thrive — not chase an arbitrary number. That means focusing on:
- Building muscle, especially in midlife and menopause.
- Protecting bone density.
- Improving cardiovascular fitness.
- Supporting hormonal balance.
- Reducing visceral fat through sustainable habits.
If we keep telling women (and men) that their worth or wellness is measured by BMI, we risk ignoring the real signs of progress — strength, stamina, confidence, and quality of life.
So Why Is BMI Still Used?
Truthfully? Convenience. It’s quick, easy, and fits nicely into insurance forms and statistical models. But in clinic, we can do better. We can use more relevant tools, ask better questions, and personalise our care.
The Takeaway
BMI isn’t useless — but it’s far from the full story. It’s time we stopped letting it dictate our definitions of health and self-worth. At Temple Clinic, we use body composition, waist measurements, and individual health goals to guide your journey — not outdated charts.
Because real health? That’s measured in strength, energy, and how you feel in your own skin.